Intrinsic factor (IF) is a secreted glycoprotein produced by the gastric Parietal cell that binds Vitamin B12 (cobalamin) and permits its receptor‑mediated absorption in the terminal Ileum. IF deficiency—acquired or hereditary—causes malabsorption of cobalamin and underlies the pathophysiology of Pernicious anemia. According to StatPearls and the NCBI Bookshelf, IF is essential for normal cobalamin uptake via ileal receptors, and its absence leads to hematologic and neurologic disease from vitamin B12 deficiency (megaloblastic anemia, neuropathy). StatPearls—Physiology, Gastric Intrinsic Factor;
StatPearls—Vitamin B12 Deficiency.
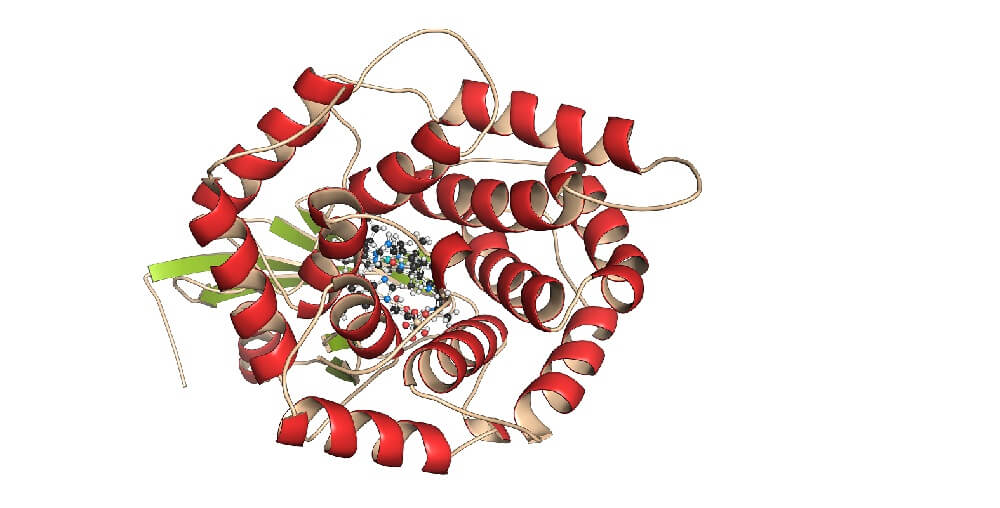
Structure and gene
- –IF is a single‑chain, secreted glycoprotein of approximately 45–50 kDa, encoded by the human CBLIF/GIF gene (HGNC:4268) on chromosome 11q12.1; the mature protein is 417 amino acids long. Protein resources and gene catalogs place CBLIF at cytoband 11q12.1 and document secretion to the gastric lumen.
Human Protein Atlas—CBLIF;
KEGG Gene hsa:2694;
GlyCosmos—P27352;
Orphanet—CBLIF.
- –The IF–cobalamin complex engages the apical multiligand receptor “cubam,” composed of Cubilin (CUBN) and amnionless (AMN); CUBN confers ligand binding and AMN anchors and mediates endocytosis. Experimental and genetic studies show that mutations in CUBN or AMN cause Imerslund–Gräsbeck syndrome, and in GIF cause hereditary intrinsic factor deficiency.
Blood—“Complex receptor for vitamin B12–intrinsic factor”;
PubMed—AMN directs endocytosis of cubam;
Orphanet Journal of Rare Diseases—genetics of inherited cobalamin malabsorption.
Physiology: secretion, binding, and absorption
- –IF is secreted by oxyntic mucosa (body and fundus) alongside gastric acid; secretion parallels acid stimulation by acetylcholine, gastrin, and histamine. Classic physiologic studies show that vagotomy or H2 blockade reduce both acid and IF, whereas secretin and the H+/K+‑ATPase inhibitor omeprazole depress acid but not IF secretion itself.
PubMed—Intrinsic factor secretion and cobalamin absorption.
- –Dietary cobalamin is protein‑bound and requires gastric acid and pepsin for release, then binds salivary/gastric haptocorrin; pancreatic proteases in the duodenum liberate cobalamin to bind IF, forming the IF–B12 complex. This complex is endocytosed in the distal ileum by the cubam receptor, and vitamin B12 then exits the enterocyte bound to transcobalamin II. Authoritative reviews and nutrient references outline this multi‑step process.
Institute of Medicine—DRI Vitamin B12;
StatPearls—Physiology, Gastric Intrinsic Factor;
PubMed review—Vitamin B12 absorption and malabsorption.
- –In adults with normal gastric physiology, roughly half of a small (food‑level) oral B12 dose is absorbed via the IF‑dependent pathway, whereas only about 1–2% of a large crystalline dose is absorbed by passive diffusion without IF; this underlies the effectiveness of high‑dose oral replacement in IF deficiency.
IOM/National Academies—DRI Vitamin B12;
StatPearls—Vitamin B12 (Cobalamin).
Molecular uptake in the ileum
- –Cubilin contains multiple CUB domains that bind IF–B12 in a calcium‑dependent manner; amnionless provides membrane anchorage and internalization signals. Human and animal studies indicate that cubilin–amnionless can mediate ileal uptake independently of megalin, which is more relevant in renal proximal tubule protein reclamation.
StatPearls—Physiology, Gastric Intrinsic Factor;
PMC—Lack of megalin in adult human terminal ileum.
Regulation, diet, and medications
- –Long‑term suppression of gastric acidity can hinder liberation of food‑bound vitamin B12 and reduce availability for IF binding, increasing deficiency risk in susceptible individuals; this has been reported with chronic acid‑reducing therapy.
StatPearls—Vitamin B12 (Cobalamin);
NIH Office of Dietary Supplements—Vitamin B12 (consumer).
- –Associations between Helicobacter pylori infection, corpus‑predominant gastritis, and impaired B12 absorption have been described, though a direct causal role in pernicious anemia remains uncertain.
StatPearls—Pernicious Anemia.
Genetics and hereditary deficiency
- –Biallelic pathogenic variants in GIF (CBLIF) cause hereditary intrinsic factor deficiency, presenting in childhood with cobalamin malabsorption despite normal gastric acid and absence of anti‑IF antibodies. Case series and gene catalogs place GIF at 11q12.1 and document diverse loss‑of‑function alleles.
BMC Medical Genetics—hereditary IF deficiency case;
Orphanet—CBLIF.
Clinical significance
- –Autoimmune loss of IF due to Autoimmune gastritis (AIG) is the most frequent cause of IF deficiency and pernicious anemia in adults. In AIG, antiparietal cell antibodies and anti‑intrinsic factor antibodies impair acid production and IF availability, leading to B12 deficiency.
StatPearls—Pernicious Anemia;
Britannica—Pernicious anemia.
- –Type I (“blocking”) and type II (“binding”) anti‑intrinsic factor antibodies are described: type I blocks B12 binding to IF; type II recognizes IF–B12 and interferes with ileal receptor binding. Classic immunochemical studies defined these specificities.
J Clin Invest—Studies on antibody to intrinsic factor;
Oxford University Hospitals—IF antibodies test.
- –Anti‑IF antibodies have high diagnostic specificity but modest sensitivity; combining anti‑IF with antiparietal cell antibody testing increases sensitivity for pernicious anemia. Contemporary reviews estimate anti‑IF sensitivity near 37–50% and specificity approaching 100%.
PMC—Optimal management of pernicious anemia;
PubMed—Autoantibodies in pernicious anemia.
- –Pernicious anemia and AIG are associated with elevated risks of gastric neoplasia, particularly non‑cardia adenocarcinoma and type 1 gastric neuroendocrine tumors; large database and meta‑analytic studies estimate roughly 2–7‑fold increased risks, though absolute annual incidences are low.
SEER‑Medicare study;
Systematic review—gastric cancer in pernicious anemia.
Diagnosis
- –Laboratory evaluation of IF‑related B12 malabsorption includes serum B12 (with methylmalonic acid and homocysteine for metabolic confirmation), anti‑IF and antiparietal cell antibodies, and, where indicated, assessment for corpus‑predominant atrophic gastritis. Clinical laboratory guidance documents the use and limitations of these assays.
Oxford University Hospitals—IF antibodies test;
ARUP—Gastric Parietal Cell Antibody.
- –The Schilling test, historically used to localize cobalamin malabsorption and demonstrate IF dependence, is now largely obsolete and unavailable in many centers.
Merck Manual Professional—Vitamin B12 Deficiency: Schilling test.
Management and replacement therapy
- –Parenteral cyanocobalamin or hydroxocobalamin reliably corrects deficiency regardless of IF status; lifelong therapy is required in pernicious anemia and congenital IF deficiency. Hematologic responses are prompt; neurologic recovery depends on duration and severity.
StatPearls—Pernicious Anemia.
- –High‑dose oral vitamin B12 (e.g., 1000–2000 µg/day) achieves adequate absorption via passive diffusion (~1–2% of dose) and is an effective alternative to intramuscular therapy for many patients, as supported by randomized trials and systematic reviews.
Cochrane Review—Oral vs intramuscular B12;
Blood—B12 deficiency perspective;
StatPearls—Vitamin B12 (Cobalamin).
History
- –The term “intrinsic factor” was introduced by William Bosworth Castle in the late 1920s to denote a gastric component necessary for absorption of a dietary “extrinsic factor,” later identified as vitamin B12. Historical accounts and classic commentaries detail Castle’s feeding experiments mixing gastric juice and meat in pernicious anemia patients.
Britannica—Intrinsic factor;
JAMA—An ‘Extrinsic Factor’ and Pernicious Anemia (historical).
- –Earlier, George H. Whipple, George R. Minot, and William P. Murphy demonstrated dramatic responses of pernicious anemia to liver feeding, work recognized by the Nobel Prize in Physiology or Medicine in 1934 and later linked mechanistically to vitamin B12 and IF.
NobelPrize.org—Minot facts;
NobelPrize.org—Murphy facts;
NobelPrize.org—Whipple facts.