Afferent lymphatic vessels are the lymphatic channels that carry lymph toward a Lymph node, entering on its convex surface through the capsule and delivering their contents to the subcapsular sinus for subsequent passage through cortical (trabecular) and medullary sinuses. They are generally more numerous than the single or few Efferent lymphatic vessels that exit at the hilum, ensuring ample delivery of tissue-derived fluid and antigens for nodal filtration and immune recognition. Kenhub;
StatPearls.
Anatomy and course
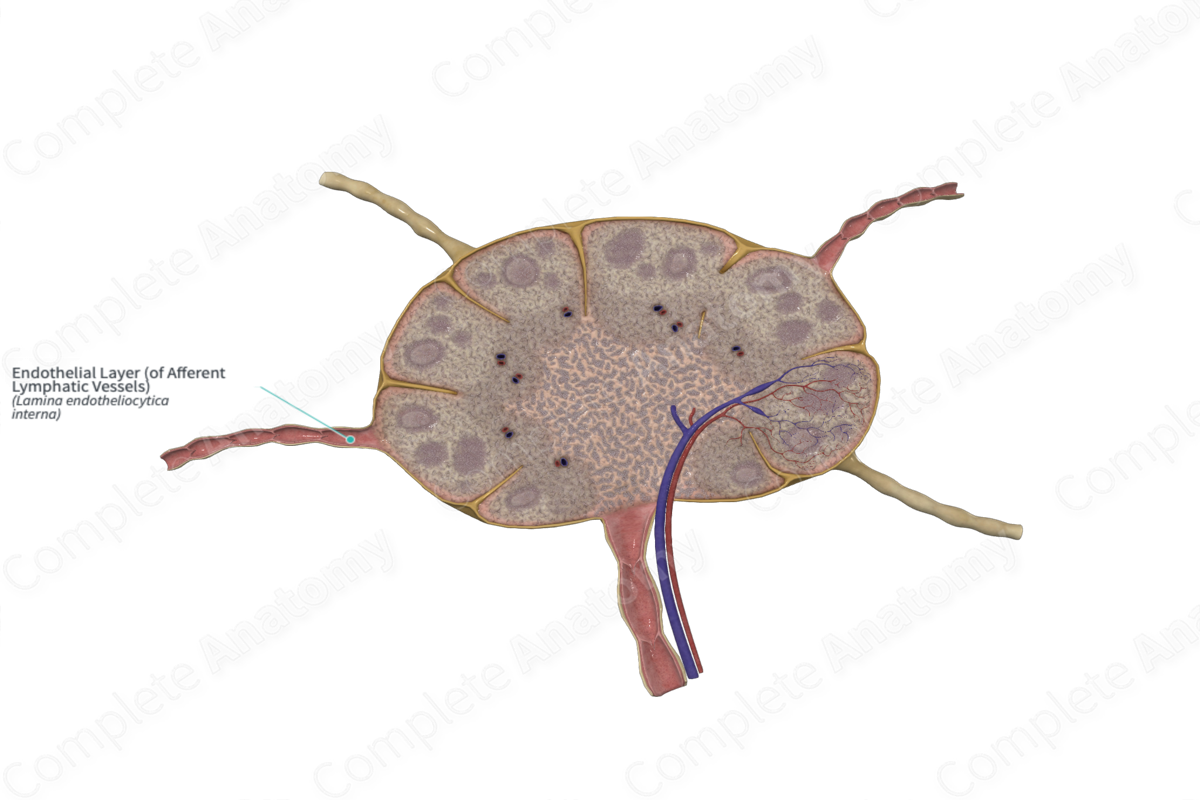
- –Entry points: Afferent vessels pierce the fibrous capsule on the convex surface of the node and open into the subcapsular (marginal) sinus that encircles the cortex. From there, lymph flows to trabecular (cortical) sinuses and then to medullary sinuses before exiting via efferent vessels at the hilum.
Kenhub;
Complete Anatomy;
StatPearls.
- –Nodal sinuses and filtration: The subcapsular, trabecular, and medullary sinuses are lined by discontinuous endothelium and supported by a reticular fiber meshwork that slows lymph transit and facilitates trapping and phagocytosis of particulate material.
Complete Anatomy;
Kenhub.
- –Numbers and distribution: Multiple afferent vessels converge on most nodes, whereas one or a few efferent vessels leave at the hilum; afferents may be peripheral collectors or internodal connections.
Kenhub;
Kenhub.
Structure and physiology
- –Vessel type: Afferent vessels approaching nodes are prenodal collecting lymphatics composed of a lymphatic endothelium supported by a basal lamina and a variably developed smooth muscle layer, with intraluminal semilunar valves that enforce centripetal flow.
NCBI Bookshelf;
StatPearls.
- –Lymphangions and pumping: Collecting lymphatics are segmented by valves into lymphangions that generate intrinsic, rhythmic contractions to propel lymph; this pumping is modulated by transmural pressure and shear stress.
American Journal of Physiology review;
PubMed;
PubMed.
- –Precollectors vs. collectors: Precollectors may contain valves with sparse or absent smooth muscle, while collectors have a continuous smooth muscle layer and valves; both feed prenodal afferents.
PubMed.
- –Development and valves: The molecular program that forms and maintains lymphatic valves (e.g., PROX1, FOXC2, GATA2) underlies unidirectional flow in collecting vessels that function as afferents to nodes.
JCI;
Frontiers in Cell and Developmental Biology.
Role in immune transport
- –Antigen carriage: Afferent vessels deliver soluble antigens and particulate material from peripheral tissues to nodal sinuses, where reticular networks and resident phagocytes promote capture and processing.
Complete Anatomy;
Kenhub.
- –Dendritic cell (DC) migration: Tissue DCs upregulate CCR7 and migrate along immobilized and soluble CCL21 gradients into afferent lymphatics and onward to draining nodes, a process central to antigen presentation in the T‑cell zone.
Frontiers in Immunology;
Journal of Immunology;
Journal of Immunology. The first entry of many DCs occurs through the floor of the subcapsular sinus, whereas some lymph-derived T cells enter from medullary sinuses, reflecting route-specific microanatomy.
PubMed.
- –Subcapsular sinus macrophages: Specialized CD169+ macrophages at the subcapsular sinus rapidly capture lymph‑borne virions and other particulate antigens delivered by afferent lymph and transfer them to B cells in follicles, aiding humoral responses.
Nature;
Blood.
Relationship to the Lymphatic system
- –Upstream sources: Interstitial fluid enters blind‑ended initial lymphatics via overlapping endothelial junctions tethered by anchoring filaments, then flows through precollectors to prenodal collecting vessels that become afferent lymphatics at the node.
NCBI Bookshelf;
StatPearls.
- –Downstream drainage: After nodal transit, lymph proceeds via efferent lymphatics to regional trunks and ultimately to the right lymphatic duct or Thoracic duct for return to the venous circulation.
StatPearls.
Distribution and exceptions
- –Lymph nodes vs. other lymphoid organs: Afferent lymphatic vessels are characteristic of lymph nodes and are absent from the Thymus and Spleen, which possess efferent lymphatics but receive antigens primarily via blood rather than via afferent lymph.
StatPearls;
PMC.
Clinical relevance
- –Metastatic spread and mapping: Many carcinomas disseminate first via afferent lymphatics to the sentinel node, underpinning sentinel lymph node biopsy in diseases such as breast and endometrial cancer.
PubMed;
MDPI;
PubMed.
- –Lymphedema: Impaired lymph transport in initial, precollector, or collecting lymphatics—including prenodal afferents—leads to chronic interstitial fluid accumulation with tissue remodeling.
StatPearls.
- –Lymphangitis: Infection and inflammation of lymphatic vessels present clinically with tender red streaks tracking proximally along afferent channels from a site of skin infection and require prompt treatment.
Cleveland Clinic.
Terminology and internal organization
- –“Afferent” denotes flow toward a node, in contrast to “efferent” (away from the node); prenodal “collecting lymphatics” function as afferents once they approach and enter the node capsule.
StatPearls;
NCBI Bookshelf.
Quantitative context
- –Whole‑body lymph return to the venous system in adult humans is generally a few liters per day at rest, driven by a combination of extrinsic tissue forces and intrinsic lymphangion pumping in collecting lymphatics.
American Journal of Physiology review;
PubMed.